Case Study
Community Health Assessments: Taking a Collective Approach
In Baltimore County, a collective approach to the traditional community health assessment helped to save money, broaden public participation, and build alignment among providers. Here’s a look behind the scenes of the countywide effort.
By Brian Ackerman
At Ascendient, our mission is strengthening healthcare delivery to ensure the best and most equitable health outcomes for all. Though we might be best known as a strategic advisor to hospitals and health systems, we also have a strong and growing client base among public health departments. We see these complementary practices as critical to our mission, and we believe that better coordination between nonprofit health systems and public health departments is a key strategy for delivering better care at lower costs.
A recent engagement in Maryland illustrates the benefits of such collaboration.
Working with the Baltimore County Department of Health (BCDH) plus all of the hospitals and health systems operating in the county, we completed a Community Health Assessment that went far beyond “checking the boxes” for this triennial chore. By bringing together the leading healthcare providers in Baltimore County, both public and private, we led a CHA process that was:
- More cost effective. Participants shared data, coordinated tasks, and aligned goals to cut down on costly duplication and overlap. We estimate that producing a single, integrated CHA saved more than $100,000 for members of the Collaborative – money that can be much better invested in health outcomes.
- More thorough and representative. By leveraging the combined networks of six Collaborative members, Ascendient was able to conduct primary research that incorporated feedback from more than 4,000 residents in every corner of the county – a larger and more geographically inclusive sample than the typical CHA budget would allow.
- Easier to implement. All too often, Community Health Assessments are little more than “wishful thinking” because communities are interdependent, and any single entity lacks the delivery mechanisms to make real change. But by uniting the hospitals that serve multiple communities, Baltimore County is better positioned to deliver health action plans that are both strategic and achievable.
What follows is a closer look the unique, coordinated effort to produce a CHA capable of making a real difference in the lives of Baltimore County residents.
Community Health Assessments in the Baltimore County Context
Occupying 612 square miles at the geographic center of Maryland, Baltimore County is home to more than 825,000 residents who are slightly older and less affluent than the state average. The county’s population is 64% White, 29% Black, and 6% Asian. Roughly 6% of residents identify as Hispanic. (All figures rounded.)
Ascendient has served as a strategic advisor to the Baltimore County Department of Health for more than a decade, with engagements that include staff training, Community Health Improvement Plans, and multiple Community Health Assessments. The County has long been proactive in including various hospital representatives on its CHA steering committee, but this latest effort represented a whole different level of commitment.
Leveraging its long relationship with Ascendient plus its strong connections in the community, BCDH was determined to include every hospital county-wide in an innovative process of data sharing, input, and feedback – all the necessary ingredients for a single, comprehensive CHA.
In addition to the Baltimore County Department of Health, members of the Collaborative included:
- Greater Baltimore Medical Center Healthcare
- MedStar Franklin Square Medical Center
- Northwest Hospital of LifeBridge Health
- Sheppard Pratt
- University of Maryland St. Joseph Medical Center
For the new effort, we started, as usual, by evaluating prior Community Health Assessments published by Collaborative members. Lacking any prior coordination, it came as no surprise when we discovered far too many priorities for a targeted approach to population health across a population as large and diverse as Baltimore County’s.
To arrive at a more manageable list, we set the goal of agreeing to just three priority areas that would allow all providers in the county to continuously measure, promote, and improve the health of the community.
Within the three large “buckets,” however, we stipulated that each Collaborative member would have the flexibility to focus on the most pressing needs in their particular sub-markets. With those parameters in mind, Collaborative members settled on the following priorities:
- Behavioral health (including mental health and substance use disorders)
- Physical health
- Health disparities
Starting from a list of more than 100 potential needs, it was no small feat to narrow the focus to these three priority areas – an achievement that was possible only with a meticulous and wide-ranging research process.
Laying the Groundwork
All Community Health Assessments require both new and existing data, but working with the Collaborative allowed primary research that reached much deeper into the community than the typical, single-client engagement. At the highest level, each member of the Collaborative appointed at least one representative to the CHA Steering Committee, creating a sort of county-wide brain trust with the widest possible view of healthcare delivery.
Working from “grass tops” to “grass roots,” we helped to design a series of research efforts, both quantitative and qualitative, to test and validate the views of the Steering Committee:
- Seventeen focus groups provided opportunities for open-ended discussion among various clusters of the broader community, including a local Baptist church, a homeless roundtable, and an LGBT community center.
- Online surveys of community health leaders provided additional expert-level input.
- Online surveys of the overall community allowed end users to provide their views of health needs and opportunities.
Rather than performing the research directly, as we typically do in a CHA engagement, in this case Ascendient simply managed the process and synthesized the findings. By empowering our Collaborative partners to engage their own communities with targeted surveys and focus groups, we were able to reach more than 4,000 residents across all geographic and demographic lines. That kind of ambitious research agenda can make a real difference, offering a much more detailed and nuanced view of health needs.
Adding It Up
After months of research, we found ourselves with hundreds of health indicators that were more interesting than they were actionable. For six Collaborative members – each with their own constituents and agendas – the sheer volume of data made it impossible to rank or prioritize the areas of greatest common need.
To bring a bit of mathematical rigor to an otherwise subjective winnowing process, we began by comparing hundreds of individual indicators against state and national benchmarks, then assigning green/yellow/red urgency levels. So, local indicators that trailed benchmarks by at least 5% were considered high need, while those scoring at least 5% better were considered low need. Any indicator within 5% of the benchmark was scored as a medium need. To give just one example:
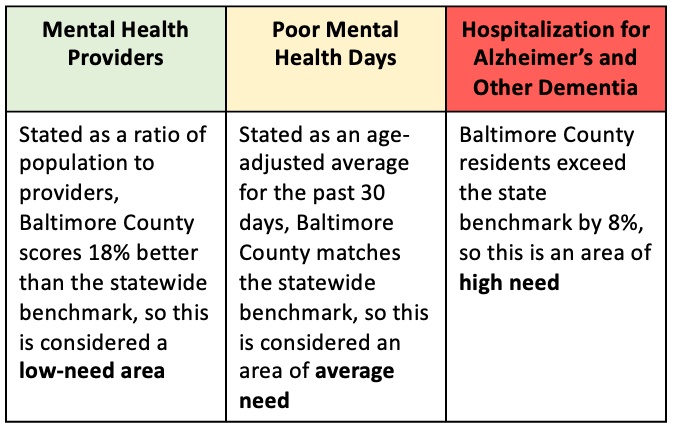
Next, we combined related indicators into broad categories for easier comparison. For instance, the three indicators above rolled up into the Mental Health category, which also included measures such as suicide and ED visits for mental health concerns. Likewise, indicators such as drug overdose deaths, excessive drinking, and opioid prescription rate were combined under the category Substance Use Disorders.
Finally, we analyzed primary research (surveys and focus groups) using these same 20 categories. In focus groups, we used open-ended questions such as, “What are the biggest problems facing this community,” then coded responses that corresponded to one of the 20 broad categories. Any response mentioned in at least seven focus groups (out of 17) was flagged as a high-need area.
For surveys, we asked multiple-choice and yes/no questions designed to
measure the perceived urgency around issues such as Access to Care, Social Supports, and Food Security. Once again, answers were coded to correspond to the 20 broad categories, which were then ranked according to frequency of response.
In the end, we found both similarities and differences in the ranking of health needs based on various types of primary and secondary research. Mental Health, Physical Health, and Access to Care consistently ranked high on the need scale, but many other categories diverged widely. For instance, the broadest community survey found high need in areas such as Safety or Social Supports, while leadership surveys ranked both of those areas as low need. Conversely, the leaders ranked Housing and Transportation as high-need areas, while focus groups discounted the urgency of such issues.
A Feature, Not a Bug
This variation in perceived need was a key finding – and perhaps a bit of a surprise to members of the Collective. Every nonprofit hospital conducts its own CHNA on a regular basis, but with a smaller service area under study, the range of identified needs tends to be narrower. Yes, there are pockets of difference between neighboring Zip codes, but nothing like the wide variance seen across a county spanning 600 square miles.
Guided by unprecedented input from every corner and every level of the community, the Baltimore County Department of Health identified health disparities that would likely never have surfaced in more traditional Community Health Assessments. Though it was sometimes tempting to see the “shotgun” pattern as a design flaw, in the end the Steering Committee recognized it as a key strength of the research – “a feature, not a bug,” in the parlance of software design.
Drilling into the data by race and geography, the Steering Committee was struck by glaring differences in access, outcomes, and perception. Of course, anyone working in healthcare knows that disparities exist, but again, the disparities are somewhat muted at the individual hospital level. By taking part in a countywide research process, hospital leaders were able to wrestle personally with the more complex range of issues facing the Baltimore County Department of Health.
Faced with the challenge of whittling down 100+ problem areas into just three county-wide priorities, the Steering Committee eventually settled on Behavioral Health, Physical Health, and Health Disparities.
Acting on its own, the Baltimore County Department of Health might have come up with the same list, but we very much doubt it would have had the same effect. Through the efforts of the Collective, every major hospital in the county is now committed to better understanding the health inequalities that plague 800,000 residents – a shared focus that might be unique in the field of public health.
At Ascendient, we’re proud of the role that we played in this groundbreaking Community Health Assessment, and we hope other health departments will be inspired to follow a similar path. We’d be happy to show you the way.
As a leading proponent of place-based healthcare, Ascendient has proudly served numerous public health departments for nearly 30 years. Please contact us to learn more about our services.
[cta 1]


Comments